Will monkeypox take the Covid-19 route?

On 23 July 2022, the World Health Organization (WHO) declared monkeypox (mpox) outbreak a Public Health Emergency of International Concern. It’s a virus that belongs to the same family as smallpox and chickenpox. The outbreak was seen in 112 countries, with a total of 87,972 laboratory-confirmed cases and 1,097 probable cases, including 147 deaths, as of 19 June 2023. And the first case in Nepal was seen recently, on June 16. This has raised several concerns among the public about the possible outbreak of mpox in Nepal. “While mpox isn’t as contagious as Covid-19 since the virus isn’t airborne, there’s still a chance that this one case might lead to an outbreak if we aren’t careful,” says Dr Prajwal Pudasaini, a dermatologist at the Civil Service Hospital, Minbhawan, Kathmandu. According to a WHO report, an infected person can transmit the virus one to four days before showing any symptoms, and until the symptoms/rashes heal. The incubation period (the number of days between the start of infection and showing of symptoms) for the mpox is around three to 17 days. The common symptoms might last two-four weeks, which include high fever, swollen lymph nodes, and rashes. It transmits sexually, through skin-to-skin contact, saliva, mucus, and pus from rashes and droplets. The symptom starts with fever and rashes appear two-three days post-fever. “It can easily be confused with common viral fever, during which people might not maintain the needed distance,” says Dr Pudasaini. Also, since many people aren’t aware of mpox, they might not opt for medical tests. He adds that some might also confuse mpox with chickenpox, not knowing the difference between the rashes. “In the case of mpox, rashes first appear on palms, feet, and genitalia, whereas chickenpox appears all over the body,” he says. The rashes in mpox are filled with mucus/pus, unlike in chickenpox. “Also, people might not stay in isolation thinking they are already immune to chickenpox,” he adds. Despite that, the possibility of an outbreak is quite minimal, especially in Nepal because virus transmission is not possible without close physical contact, says Dr Janak Koirala, professor of infection disease/internal medicine at Patan Academy of Health Sciences (PAHS). “Since the first case was quickly identified, it might not have spread in a group,” he says, “But it’s necessary to follow the infected’s travel history, as well as trace and monitor her contacts.” Dr Rudra Marasini, director, Epidemiology and Disease Control Division (EDCD) under the Ministry of Health and Population (MoHP), says that the 60-year-old infected individual’s contacts have been traced and they are under close observation. “She had a travel history, and we have managed to contact everyone who came into contact with her within the 21 days prior to when her symptoms appeared,” he says. So far, only one of the contacts has shown signs of mpox, but the test result came out negative. Dr Hemanta Chandra Ojha, section chief, Zoonotic and Other Communicable Disease Control Section, EDCD, says other contacts haven’t shown any symptoms of mpox thus far. They will be under observation until the incubation period is over. “Since the illness didn’t originate in Nepal, it’s highly unlikely that this will turn into an outbreak,” he says. But to remain prepared, Dr Marasini mentions that medical professionals in Nepal have received training on dealing with cases of mpox. “We have 14 sites all over Nepal where professionals trained in handling mpox have been stationed,” he says. Dr Dharmendra Karn, a dermatologist, says most healthcare professionals began keeping themselves updated with the mpox virus after an outbreak in 2022. “We didn’t know when it would enter Nepal, so we have always stayed prepared,” he says. Also, for most individuals, the symptoms are only limited to fever and skin rashes, unless they are immuno-compromised. “It might prove to be fatal for infants, elderly and pregnant individuals, as well as people with chronic illnesses like diabetes, existing heart and liver issues, and HIV/AIDS,” says Dr Karn. In these cases, mpox might lead to other complications like meningitis, encephalitis, pneumonia, and organ failure. However, the mortality rate, so far, is less than one percent globally. “Much depends on the type of mpox variant,” says Dr Pudasaini. There are two variants of mpox prevalent globally—Central African (Clade I) and West African (Clade II). Among them, Clade II doesn’t cause much severity, whereas, according to Pudasaini, Clade I is thrice as lethal as the omicron virus. “Not knowing what variant we are dealing with, we can’t be sure on what the outcome might be,” he says. Nevertheless, the 2022 outbreak was caused by the subtype of Clade II called Clade IIb, which isn’t as severe as Clade I. Unfortunately, Nepal doesn’t have the mechanism to identify mpox variants. The best thing to do at the moment, Dr Karn believes, is to go back to the preventive measures everyone took during the Covid-19 pandemic. “We need to start maintaining distance, wearing masks, and using sanitizers,” he says. He adds that it’s necessary to inform people on the possible symptoms of mpox and precautions to take when one shows signs of infection. “Many people don’t even know what mpox is,” he says. Dr Koirala says it’s important to prevent the virus from reaching places like hostels, schools, and workplaces, where there is close contact. “It’s also transmissible from towels, clothes, utensils, and items used by the infected,” he says. If found in places where people remain together in a cluster for long hours, an outbreak cannot be prevented. But if there is an outbreak, doctors and medical professionals ApEx spoke to believe that Nepal’s healthcare system is well-equipped to handle it. “Many hospitals now have good isolation wards, ICUs, and have a good knowledge on dealing with medical crises,” says Dr Santa Kumar Das, deputy director, Tribhuvan University Teaching Hospital at Maharajgunj, Kathmandu. But there are a few improvements needed, like increasing the number of labs that conduct Polymerase Chain Reaction (PCR) tests for mpox. Currently, the test is only available at the National Public Health Laboratory (NPHL) in Teku. To prevent the virus from making inroads into the country, a proper screening system must be put in place to know whether a person is suffering from mpox, experts say. “The best way is to prepare a screening questionnaire, and send individuals showing symptoms for a PCR test,” says Dr Koirala. For now, the MoHP has stationed trained individuals at airports to perform proper screening. “We are doing everything we can to prevent the virus from entering the country,” says Dr Marasini. Data: Countries with maximum mpox cases since the 2022 outbreak, as of 6 June 2023
| Country | Cases | Deaths |
| Aruba | 30,468 | 0 |
| Andorra | 10,948 | 0 |
| United Arab Emirates (UAE) | 7,556 | 0 |
| Argentina | 4,146 | 2 |
| Australia | 4,090 | 0 |
| Austria | 4,020 | 0 |
| Belgium | 3,800 | 2 |
| Benin | 3,753 | 0 |
| Bulgaria | 3,691 | 0 |
| Bahrain | 1,496 | 0 |
Source: Centers for Disease Control and Prevention (CDC) Symptoms Fever Rashes first appear on the palm, feet and genitalia two-three days post fever. Pus/mucus filled rashes appear all over the body Swollen lymph nodes Control measures Maintain physical distance Wear mask Use sanitizer Raise public awareness on the disease
related news
Lumpy skin disease and its economic impact
July 10, 2023, 6:17 p.m.
Silver lining for Pancheshwar project
July 10, 2023, 6:05 p.m.
Private sector’s boost may spur economic rebounding
July 7, 2023, 4:47 p.m.
Three-way competition and Nepal
July 5, 2023, 4:28 p.m.
The unaccounted costs of a self-focused mindset
July 5, 2023, 1:49 p.m.
Nepal should adopt a multi-alignment policy
July 4, 2023, 11:36 p.m.
White man’s burden, brahminism and racial superiority
July 4, 2023, 6:05 p.m.
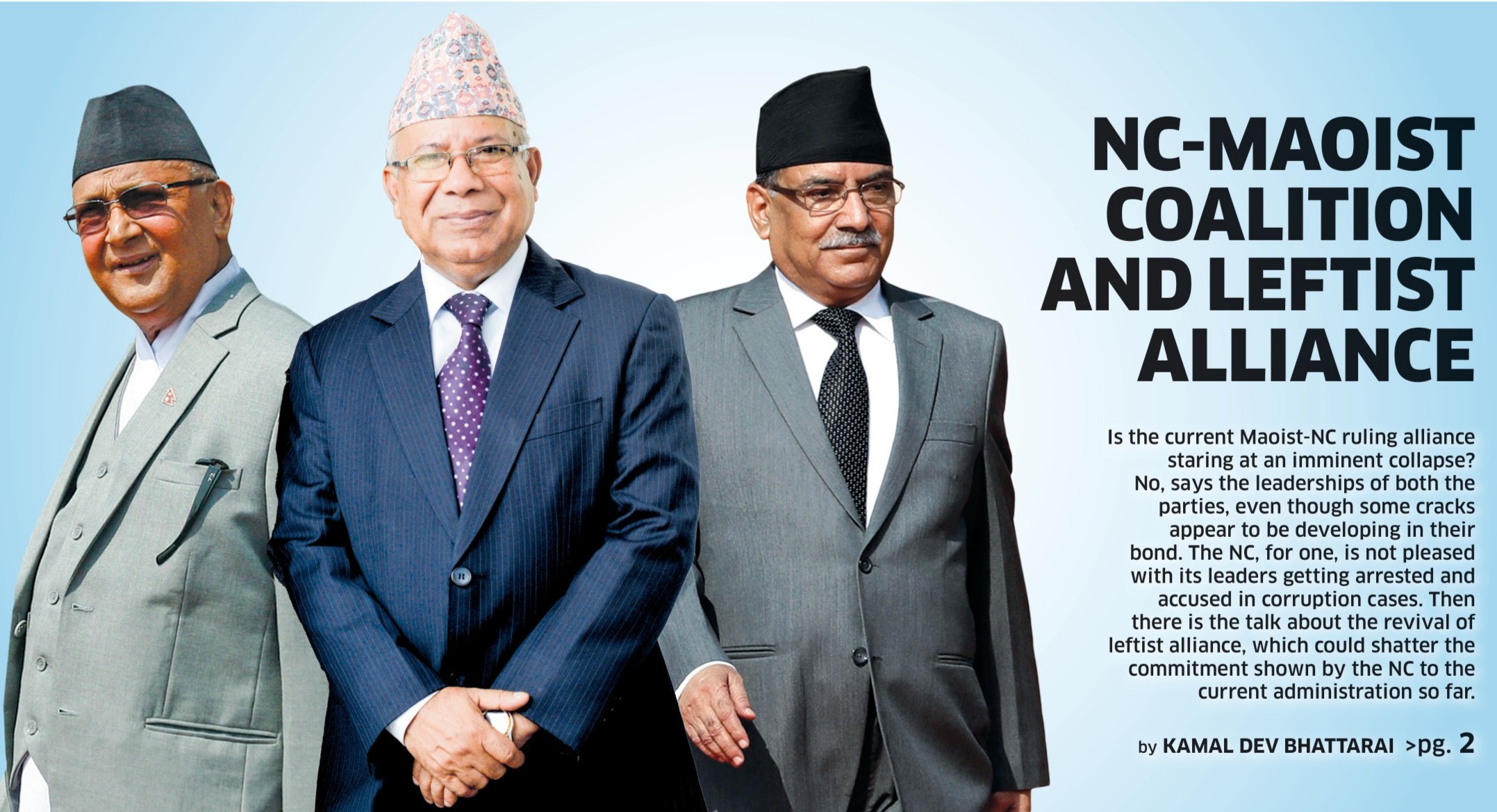
Is ‘left unity’ on the card?
July 4, 2023, 2:44 p.m.









Comments