A holy river or a health hazard?
The Bagmati river is revered as a sacred lifeline, deified for its purifying waters and deeply entrenched cultural and religious significance. It serves as a ritual site for cremation and spiritual cleansing in the pursuit of salvation, embodying the belief that its sacred flow can absolve karma and unite the soul with the divine, forming a transcendent cycle where birth, death and eternity converge.
Flowing through the heart of Nepal’s Kathmandu valley, the Bagmati is more than just a body of water, it’s a sacred thread woven into the spiritual, cultural and ecological fabric of the nation. Revered in both Hindu and Buddhist traditions, it has for centuries been a symbol of civilization, sanctity and continuity, a giver of life and a pathway to salvation.
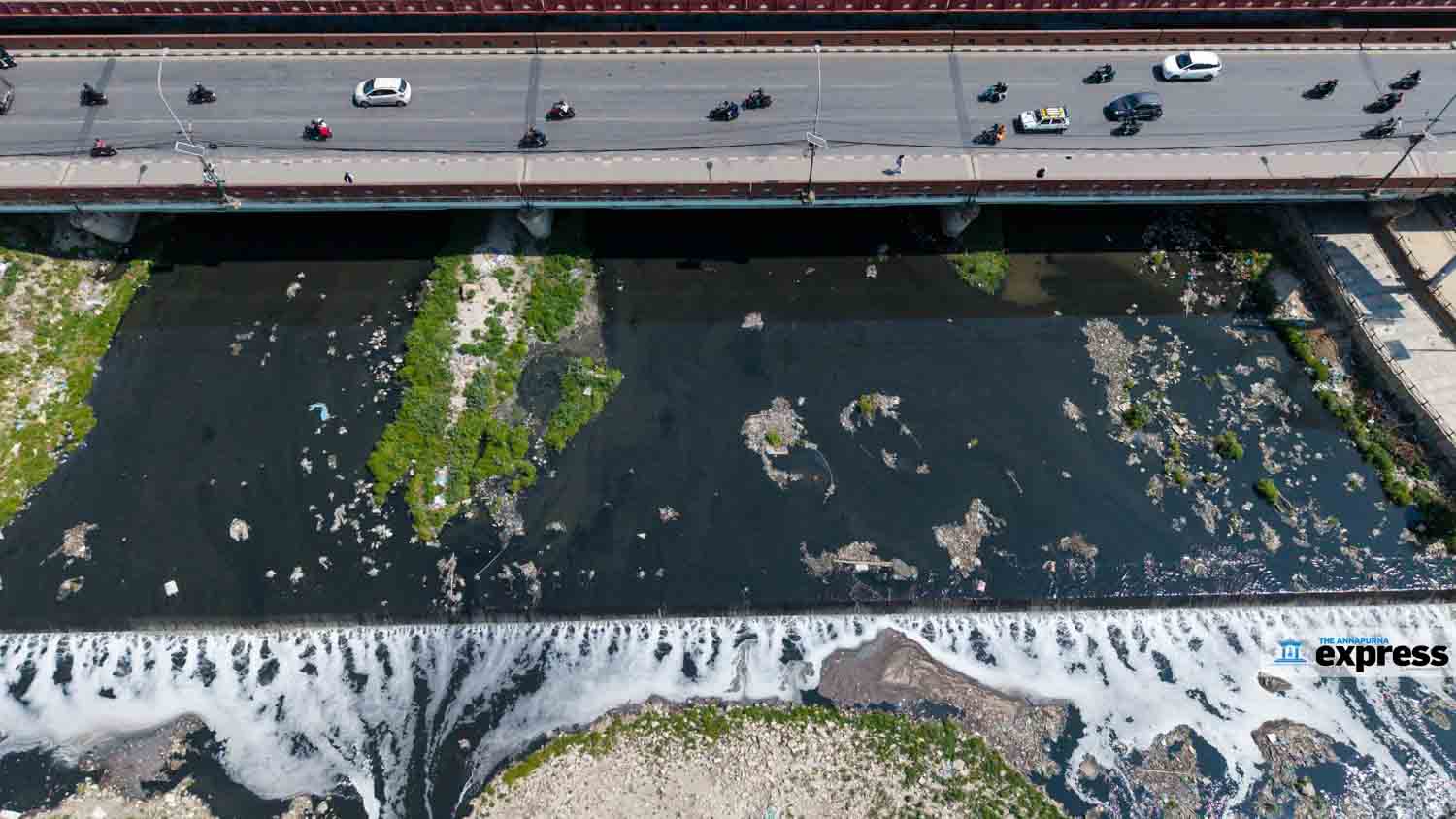
Yet today, the same river that once nourished an entire valley has been reduced to a toxic sewer. Its waters are blackened by sewage, choked with industrial waste and biohazards, and fouled by an unbearable stench. In its putrid current lies a haunting question: Can the Bagmati still be called holy or has it become a public health hazard?
Sacred shrine to sewer stream
The Bagmati river originates from Bagdwar in the Shivapuri Hills of the Mahabharat range at an elevation of 2,690 meters, where it once flowed crystal clear, pure, life-sustaining and revered. It travels southward through the Kathmandu valley (15 percent basin area), descending into the Tarai plains through eight districts before crossing into India to merge with the Ganges. For Hindus, the Bagmati is more than a river, it’s the earthly embodiment of the divine, intimately linked to Lord Shiva at the Pashupatinath Temple, a UNESCO World Heritage since 1979, where its waters are believed to carry souls toward moksha (liberation).
The river, steeped in legend and divine embodiment. According to mythology, the Bagmati began flowing when Bodhisattva Manjushree cleaved the hills surrounding a primordial lake, draining it and making way for human settlement. This act gave birth to the ancient city of Manjupattan on its banks. The Bagmati has served as a spiritual and cultural lifeline shaping early Kathmandu and marking historical trade routes at Teku Dovan and cremation sites such as Kalmochan and Pachali Ghat preserving 3,000 years of ritual heritage and royal legacy.
Today, however, the Bagmati paints a very different picture. Its once-pristine waters are choked with industrial effluents, raw sewage and biohazardous waste, primarily via anthropogenic pressures. A 2017 UN report estimated that over 95 per cent of wastewater in the valley is discharged untreated into natural water bodies much of it ending up in the Bagmati. This unchecked pollution now poses a grave hazard to both environmental and public health hindering water reuse and ecological sustainability.
The riverbanks, once adorned with temples and terraced greenery, are now strewn with plastic bags, decaying waste and the remnants of discarded ritual offerings. Despite the presence of existing and rehabilitated wastewater treatment plants, their capacity remains woefully inadequate to handle the overwhelming waste burden. Key degradation contributors are unmanaged urbanization, indiscriminate waste disposal and the direct discharge of domestic and industrial sewage further exacerbated by poor planning, fragmented governance and the rapidly growing valley population, now nearing 3m. Unlike artificial canals, the Bagmati is a natural river, whose sandy riverbed has been stripped bare by decades of toxic dumping. Though efforts to clean and preserve the river are urgent, the prospect of restoring it to its former sanctity is uncertain. In many respects, the damage may already be irreversible.
Health hazard—a nightmare
The Bagmati river now embodies a profound ecological and public health crisis. Scientific studies have revealed alarming levels of microbial and chemical contamination. A 2019 study published in the journal ‘water’ identified 709 bacterial genera in the river, including 18 potentially pathogenic such as Arcobacter, Acinetobacter and Prevotella. Thakali et al (2020) further detected reservoirs of antibiotic resistance genes (ARGs), transformed the Bagmati as a hotspot for antimicrobial resistance (AMR). Shrestha et al. (2023) reported that 80 per cent of river microbial isolates possessed multidrug resistance, while Ghimire et al. (JNHRC 2023) confirmed 241 of 615 coliform samples were resistant to common antibiotics.
Beyond microbial threats, a 2015 study estimated that 70,000 plastic micro- and macro-fragments pass through the river daily. Recent analyses have detected heavy metals like lead and mercury, and carcinogenic compounds capable of causing neurological damage, developmental disorders and organ failure. Despite Nepal’s abundant freshwater sources, cities like Kathmandu suffer from water scarcity. The World Bank 2016 reported 19.8 deaths per 100,000 in Nepal are linked to unsafe sanitation, hygiene and waterborne diseases. The environmental collapse is stark: fish stocks have vanished, aquatic birds are gone, and sludge, algal blooms and chemical foam dominate the landscape. Its decline is a warning not only for Nepal but for the world, a reminder that environmental neglect has irreversible consequences.
Revival possible?
Since 2013, the weekly Bagmati Clean-Up Campaign has mobilized volunteers and raised public awareness, but these efforts remain inadequate against the overwhelming scale of pollution and ecological decline. While new wastewater treatment plants are under construction, the pace of infrastructure development continues to lag behind escalating contamination levels. Legal frameworks to penalize polluters do exist, yet enforcement is weak, and often symbolic. What is urgently needed is a strict implementation of environmental laws, holding industries and hospitals accountable through regular audits and real-time monitoring. Solutions like bioremediation with pollutant-degrading microbes, installation of plastic traps at drainage outlets and widespread adoption of household waste segregation must be prioritized. Equally vital is mobilizing spiritual leadership: religious figures can champion environmental stewardship as a sacred duty and promote eco-conscious rituals.
The Bagmati mirrors Nepal’s soul, sacred, yet deeply wounded. Its revival lies not in miracles, but in unified action, scientific innovation and spiritual responsibility.
A nation that kills its rivers kills its own future. The Bagmati’s fate rests in our hands.
Measles outbreaks: High price of vaccine hesitancy
“Misinformation or distrust of vaccines can be like a contagion that can spread as fast as measles.”
– Theresa Tam, chief public health officer, Canada
In an age of unprecedented medical advancement, the resurgence of measles, a disease once nearing global elimination, is both disheartening and alarming. It stands as a stark reminder that scientific breakthroughs alone cannot defeat disease; public trust and unified action are equally essential. Measles, a highly contagious illness, had been declared eliminated in the United States in 2000 and in several European countries by 2016, following decades of successful immunization campaigns. Yet today, outbreaks are surging across globally.
This resurgence is not due to a failure in medical science, but rather a growing crisis in public perception fueled by misinformation, distrust in health systems and increasing complacency. Despite the proven safety and effectiveness of vaccines like the MMR (measles, mumps, rubella), vaccine hesitancy has weakened herd immunity, allowing the virus to spread rapidly, especially in under-vaccinated populations. In essence, fear and falsehoods have become nearly as infectious as the disease itself.
According to the US CDC, measles is an acute viral respiratory illness marked by high fever, cough, runny nose, red eyes and red rash appearing 7–14 days after exposure. It’s caused by a single-stranded, enveloped RNA Morbillivirus virus, with humans as its only natural hosts. Measles spreads through respiratory droplets when an infected person coughs or sneezes. Up to 90 percent of susceptible individuals in close contact with an infected person can get infected. The virus can remain airborne or survive on surfaces for up to two hours, making transmission possible even after the infected person has left the area.
While measles can affect varied ages, it poses the highest risk to infants and children under five and immunocompromised (pregnant women, leukemia, HIV-infected) individuals. Complications include ear infections and diarrhea, while severe complications include pneumonia, encephalitis and death. Out of every 1,000 children infected with measles, up to three die due to respiratory or neurological complications.
Laboratory confirmation is key for diagnosing sporadic measles cases and outbreaks. Diagnosis typically involves detecting measles-specific IgM antibodies in serum and RNA via RT-PCR in respiratory specimens. Collecting serum and nasopharyngeal swab at the first patient contact is recommended. Viral molecular genotyping aids in tracing transmission and distinguishing between wild-type infections and vaccine-related rashes, thereby playing a vital role in outbreak control and epidemiological surveillance.
Global reawakening
Despite the availability of a safe and affordable vaccine, measles remains a serious global health threat. In 2023, the WHO reported 10.3m measles cases globally, with an estimated 107,500 deaths, primarily among unvaccinated or under-vaccinated under-fives. In India alone, measles claims around 49,000 young lives each year. The European Region experienced its highest case count in over 25 years, with 1.27 lakh hospitalizations reported in 2024. Romania recorded 30,692 cases amid low vaccine coverage (62 percent), while Kazakhstan reported 28,147 cases with coverage below 80 percent. Notably, Kazakhstan’s measles cases surged from just four in 2010 to over 28,000 in 2024. According to Akhmetzhanova et al., 35 percent of Kazakhstani respondents expressed vaccine hesitancy, with 22 percent wrongly linking vaccines to autism, undermining immunization efforts and endangering vulnerable populations.
In the US, as of April 17, 800 measles cases were confirmed across 25 states, threefold higher than in 2024. Ten outbreaks were reported, with 94 percent of cases outbreak-associated. Alarmingly, 96 percent of infected individuals were unvaccinated or of unknown status. Texas was the hardest hit with 597 cases, largely in undervaccinated communities. Tragically, two unvaccinated children in Texas and one adult in New Mexico died from measles complications.
Historically, measles has caused devastating pandemics. In 1529, an epidemic in Cuba killed two-thirds of the indigenous population that survived smallpox. In 1531, half of Honduras’ population was wiped out by the measles epidemic, underscoring the deadly legacy of measles when vaccination rates faltered.
Resurgence in Nepal
From January to August 2023, Nepal recorded 1,013 measles cases, a tenfold increase compared to 2017. The highest case counts were reported in the Tarai. Although Nepal achieved 90 percent MMR vaccine coverage by 2019, the Covid-19 pandemic disrupted routine immunization, contributing to a resurgence in 2023–2024.
Vaccine hesitancy
Globally, measles vaccination has prevented over 60m deaths between 2000 and 2023. To achieve herd immunity, the CDC recommends 95 percent coverage with two MMR doses, administered at 12–15 months and 4–6 years of age. However, between 2000 and 2017, global two-dose MMR coverage plateaued at just 67 percent, far below the threshold needed to prevent outbreaks.
Despite its 97 percent effectiveness and proven safety, MMR vaccine hesitancy remains a formidable challenge. Defined as the delay or refusal of vaccination despite availability, hesitancy stems from cultural beliefs, misinformation, distrust and socioeconomic barriers. A key driver is the debunked Lancet study (Wakefield et al 1998) falsely linking MMR to autism. Although retracted in 2010 for ethical violations and debunked by multiple large-scale studies, its impact endures, amplified by social media.
As the saying goes, “A lie can travel halfway around the world while the truth is still putting on its shoes.” Common myths “natural immunity is better” or “vaccines contain harmful chemicals” continue to circulate, despite evidence that measles can be life-threatening and vaccine ingredients are safe and rigorously tested.
Achieving 95 percent MMR coverage is vital, not only for individual protection but also to safeguard those who can’t be vaccinated due to age or medical reasons. Herd immunity limits the spread of measles, preventing large-scale outbreaks.
Nepal has made progress in expanding immunization, yet challenges remain, particularly in remote and underserved areas. To improve coverage, Nepal must disseminate evidence-based authentic information to counter misinformation, engage local communities to build trust and strengthen policy measures, including school-entry vaccination requirements.
As the saying goes, “Vaccines don’t save lives; vaccinations do.” A sustained, multipronged approach is essential to safeguard vulnerable populations and prevent future outbreaks.
Invasive alien species: Growing global perils
“Look closely at nature. Every species is a masterpiece, exquisitely adapted to the particular environment in which it has survived. Who are we to destroy or even diminish biodiversity?” The quote by EO Wilson, a pioneer biologist, emphasizes the intrinsic value of every species and its role in maintaining biodiversity and ecosystem balance. All species, including humans, are integral to the web of life, each contributing to ecosystem resilience. As humans, we hold immense power over nature, yet this power comes with the responsibility to protect biodiversity rather than diminish it.
Our actions, such as habitat destruction and the spread of invasive species, disrupt ecosystems and threaten our own survival, highlighting the ethical imperative to preserve the intricate interdependence of life.
Invasive alien species (IAS) are non-native organisms introduced to new habitats through human activities, intentionally or accidentally, that disrupt ecosystems and threaten biodiversity. Without natural predators, IAS often proliferate rapidly, outcompeting native species and driving them to extinction. Their spread causes irreversible biodiversity loss, alters ecosystem services and incurs colossal economic and social costs. Globalization, trade, travel and climate change have further accelerated IAS spread, making them one of the top five drivers of biodiversity loss, contributing to native species extinction, noted by IPBES, 2019. Globally, around 37,000 IAS are established.
Pyšek et al (2020) reported that around 14,000 species with established alien populations represent four percent of global flora, while 175 terrestrial gastropods as IAS across 56 countries, 745 of 15,000 freshwater fish species, and 971 out of 2000 bird species have become established IAS across various regions.
Growing global perils
IAS are major drivers of biodiversity loss and native species extinction, often referred to as ‘biological pollution’ or ‘green cancer’ (Olson, 2006), while also posing risks to human health, food security and livelihoods. For example, the brown tree snake (Boiga irregularis) led to the extinction of 10 bird species on Guam after its introduction in the 1940s. The IAS Asian tiger mosquito (Aedes albopictus) spreads diseases—Dengue, Chickungunya, and West Nile virus, affecting millions globally. Water hyacinth (Eichhornia crassipes), native to South America, introduced for ornamental purposes across the world, invades water bodies, irrigation channels and rice paddies, causing ecological and economic calamity. IAS disrupt critical ecosystem services such as pollination, water purification and soil fertility, essential for natural cycles. Their spread, accelerated by global trade and travel, worsens these risks, undermining public health and economic resilience.
Economic toll associated with IAS is staggering. A study by Diagne et al (2021) in Nature estimated biological invasions have caused a minimum global economic cost of $1.288trn between 1970 and 2017. According to the IUCN, IAS cost €12.5bn annually and Australia AUS$13.6bn each year. Invasive insects alone account for $70bn in global annual losses. IAS damages agriculture, reduces fishery yields, and disrupts urban areas, leading to financial losses and increased management costs. Prominent IAS in the US, including the spotted lanternfly, red fire ant, feral swine, Emerald ash borer,
Asian carp and Burmese python, purple loosestrife, Japanese honeysuckle, barberry, English Ivy and Kudzu have altered ecosystems and incurred billions of dollars in control efforts and lost productivity. IAS like zebra mussels, native to the Caspian Sea, damage aquatic ecosystems, while the Spanish slugs devastate crops in Europe with massive economic damage.
Furthermore, IAS threaten food security and livelihoods, hindering progress toward the UN's SDG 15 aiming to protect life on land and below water. The IUCN Red List of Threatened Species (2022) reports that one in ten species on the list are threatened by IAS, emphasizing the urgent need for coordinated global efforts to mitigate their spread protecting ecosystem resilience.
The context of Nepal
IAS pose escalating threats to Nepal’s ecology, economy, sustainable development and health, reflecting global concerns. IAS in Nepal have a long history, with Chomolaena odorata (Siam weed) first reported in 1825. Known locally as ‘Banmara’, these species disrupt ecosystems, outcompete native species, and threaten agricultural productivity. An estimated 219 alien flowering plant species in Nepal’s forests, with 30 flora species are common IAS (Yadav et al, 2024). Budha 2014 reported 69 fauna species; insects (21), fish (16), birds (three), wild mammals (two), freshwater prawn (one), platyhelminthes (one) and livestock breeds (25 improved breeds), identified as common IAS. These species are primarily from the Americas (74 percent), Europe (one percent) and Africa (eight percent) and cause irreparable harm to ecology.
The introduction of IAS is driven by increasing tourism, trade and limited institutional biosecurity capacity, including insufficient policies and quarantine facilities. These conditions provide a conducive environment for exotic species. Notable flora IAS are Ageratina adenophora, Chromolaena odorata, Eichhornia crassipes, Lantana camara, and Mikania micrantha. Specifically, C odorata, E crassipes, L camara and micrantha are listed among the world’s worst IAS. Tomato leaf miner (Tuta absoluta) and Fall armyworm (Spodoptera frugiperda) harm crops, and giant African snail (Achatina fulica) spoils vegetables.
The economic cost of managing IAS, such as Tilapia in water bodies, water hyacinth in the Fewa Lake, and Mimosa diplotricha in Jhapa’s community forests, is substantial, requiring extensive resources. However, the ecological, evolutionary and economic impacts of IAS remain under-studied, with a lack of evidence-based management strategies. While physical removal is common, bio-controls have yet to be formally implemented.
Nation-wide surveys, standardized guidelines, policy-advocacy and community awareness are warranted to address IAS.
IAS pose a silent threat, eroding biodiversity and economic stability globally. While developed nations combat established invaders, countries like Nepal face escalating risks due to weak biosecurity defenses and increasing climate change concerns. Proactive measures including stronger policies, scientific research and global cooperation are essential to mitigate these growing perils. Without urgent action, the ecological and economic consequences will be irreversible.
As Wilson’s call to action reminds us, we must reconsider our role as biodiversity stewards and safeguard ecosystems for future generations. Addressing the critical challenges from IAS requires proactive policies, enhanced cross-cutting research and stronger multi-stakeholder engagement to prevent further damage to the nation’s rich biodiversity.
The author is a biological scientist
Human-wildlife interactions: Conflict to coexistence
For over 2600 years, Gautam Buddha’s moral principles have emphasized non-violence and respect for all living beings, recognizing all flora and fauna as sentient and capable of suffering. This ethos of compassion still influences Nepal’s cultural and spiritual approach to wildlife. However, modernization, habitat encroachment, climate change and anthropogenic pressures have escalated human-wildlife conflicts (HWC). As landscapes shrink, peaceful coexistence demands blending traditional ecological wisdom with science-based strategies. Achieving this harmonious balance honors Buddhism philosophy while ensuring ecological sustainability.
History: Harmony to conflict
For millennia, human societies coexisted with wildlife in a delicate balance. According to Fabrice Teletchea’s book ‘Animal Domestication (2018)’, early modern humans (Homo sapiens) emerged approximately 200,000 years ago, depended on hunting wild animals and gathering plants for survival. This dynamic began to shift around 12,000 years ago with the advent of agriculture in regions (Fertile Crescent, China and Mesoamerica). The domestication of plants and animals, coupled with agricultural expansion, progressively confined wildlife to fragmented habitats. As agrarian societies displaced hunter-gatherer communities, human-wildlife interactions (HWI) evolved from coexistence to competition.
This transition further accelerated with industrialization and urbanization. A peer-reviewed study, published in Biological Reviews, estimates that since 1500, up to 13 percent of known species—approximately 150,000 to 260,000—may have already gone extinct. This alarming loss termed “biological annihilation” is directly linked to human activities. Historical records by the Smithsonian Institute highlight species like dodo (1690), Labrador duck (1870), Tasmanian tiger (1936), Hawaii chaff flower (1962) and Golden toad (1989), all driven to extinction by anthropogenic pressures.
HWCs in Nepal
Nepal’s HWC trajectory closely mirrors global patterns. The establishment of 12 national parks and several conservation areas including Chitwan and Bardiya National Parks initially provided wildlife with critical refuge. However, these protected areas also created conflict hotspots along their buffer zones, where human settlements and agricultural lands directly border wildlife habitats.
A 2016 PLOS One Journal study documented 463 conflict incidents resulting in human injury or death caused by large mammals between 2010 and 2014. Between 2000 and 2020, Nepal recorded 1139 cases of wildlife mortality and 887 human fatalities linked to HWCs. Notably, thousands of people and their properties in the Tarai regions were affected by elephant-related conflicts alone, underscoring the gravity of the issue.
HWC refers to harmful encounters where wildlife threatens human safety, livelihoods or cultural values, often triggering retaliatory actions. HWI is a neutral term covering positive, negative or benign forms of contact. Coexistence, however, is a balanced state where humans and wildlife share space with tolerable impacts, supported by adaptive management, cultural acceptance and mutual benefits.
Nepal offers an ideal case for better understanding these dynamics. Rapid, unplanned urbanization and intensified agriculture have escalated competition for habitat and resources. Protected areas, surrounded by settlements, have led to wildlife frequently venturing into croplands and communities, heightening conflict potential.
HWC, alongside zoonotic diseases, poses significant public health risks. With 75 percent of emerging infectious diseases being zoonotic and 70 percent originating from wildlife, addressing these challenges is crucial. Deforestation, habitat fragmentation and wildlife trade create “spillover hotspots,” enabling pathogens to circulate in the wildlife-livestock-humans interface.
Forest-edge communities face heightened risks from diseases like brucellosis, leptospirosis, leishmaniasis, rabies, tuberculosis and anthrax. Wildlife are equally vulnerable to ‘reverse spillover’ reported canine distemper virus and tuberculosis in Nepal’s wild species.
Covid-19 pandemic and other outbreaks (Mpox, Ebola) highlighted the global consequences of poorly managed HWI, underscoring the urgency of integrating public health into conservation strategies to mitigate such risks.
Climate change exacerbates these risks by altering species distributions, habitat and migration patterns. Shifting temperature and precipitation disrupt wildlife foraging and breeding, pushing into human-dominated landscapes for searching for food and water. Concurrent habitat degradation reduces natural food supplies, intensifying crop raiding and livestock predation. Nepal, a biodiversity hotspot, is vulnerable to these cascading effects. The keystone species loss and ecosystem disruptions jeopardize the ecology essential for wildlife and local livelihoods.
Policy landscape
Nepal’s policy response has evolved to resolve the HWC interconnected challenges, zoonotic diseases and biodiversity loss. Adoption of ‘One Health Strategy 2019’ and ‘National Wildlife Health Action Plan 2023-2032’ aim to strengthen wildlife disease surveillance, conservation medicine, and inter-agency coordination. These policies establish a framework for managing risks at the human-animal-environment interface through an interdisciplinary lens.
However, challenges remain in implementation, including fragmented disease surveillance within protected areas and limited diagnostic capacity. Institutional silos among conservation, veterinary and public health authorities hinder real-time data sharing and coordinated responses. This impedes Nepal’s ability to proactively manage health threats at the interface.
Empowering local communities in buffer zones as frontline stakeholders is key to managing HWC. Residents, bearing the brunt of HWC, possess invaluable traditional ecological knowledge, including indigenous practices like crop guarding, seasonal land-use rotation and wildlife behavior interpretation. Strategies such as electric fences, predator-proof corrals and planting wildlife-unpalatable crops (peppermint) are effective. However, science-based, species-specific and landscape-specific conflict management strategies are recommended for more sustainable solutions.
Community-managed buffer zones around Chitwan National Park demonstrate how conservation can be economically beneficial through eco-tourism. Such incentives foster stewardship, transforming wildlife from threats to valued assets.
To shift from reactive conflict management to proactive coexistence, Nepal must invest in wildlife health surveillance, community resilience and economic incentives such as compensation schemes and eco-tourism revenue-sharing. This transition needs interdisciplinary collaboration, community awareness and effective policy into action.
Integrating the Buddhist philosophy, which emphasizes respect for all living beings and their freedom from suffering, can foster behavioral changes transforming HWC into opportunities for coexistence.
Bioterrorism: The looming invisible peril
“Shall We All Commit Suicide?” Sir Winston S Churchill ominously warned in his 1924 essay about the alarming progress of biological warfare (BW), where engineered diseases could target humans, animals and agriculture. He wrote, “A study of Disease—of Pestilences, methodically prepared and deliberately launched upon man and beast—is certainly being pursued in the laboratories of more than one great country. Blight to destroy crops, Anthrax to slay horses and cattle, Plague to poison not armies only but whole districts—such are the lines along which military science is remorselessly advancing.” A century ago, Churchill predicted the risks of bioterrorism, foreseeing military strategies using engineered bioweapons that could devastate humanity and ecosystems.
In an op-ed for Business Insider in 2017, Microsoft founder and billionaire philanthropist Bill Gates warned “Infectious virus is a greater risk to humanity than nuclear war. Whether such an outbreak occurs due to a quirk of nature or is deliberately released by a terrorist, epidemiologists say a fast-moving airborne pathogen could kill more than 30m people in less than a year.” Gates emphasized the cataclysmic gravity of BW agents, indicating bioterrorism—the deliberate release of natural or engineered biological agents to harm humans, animals, or environments for terrorist purposes—could become one of humanity’s greatest perils.
Historical perspective
BW dates back to the 6th century BCE when the Assyrians poisoned enemy wells with ergot fungus, causing delusions, cardiovascular issues and death, and has since been a strategic tool in military conflicts. In the 4th century BCE, Scythian archers dipped arrows in animal feces to induce infections, while in 204 BCE, Hannibal used venomous snake-filled clay pots against Pergamene ships. In 1346, the Tatars catapulted plague-infected corpses into Kaffa, contributing to Black Death’s spread across Europe, which killed up to 200m people in the 14th century alone, wiping out nearly half of Europe's population.
During the 16th century, Spanish conquistadors used smallpox-infected blankets to devastate indigenous South American populations. The industrial revolution advanced microbiology, inadvertently enabling the weaponization of pathogens. During World War I, Germany allegedly infected enemy livestock with anthrax.
During World War II, Japan’s Units 731 and 100 weaponized pathogens like B anthrax, Yersinia pestis, V cholera and Shigella in ceramic bombs, dispersing them over Chinese cities via aerosols and testing them on prisoners, causing epidemics and an estimated 10,000 prisoners’ deaths.
The Cold War saw further advancements, with the United States and the Soviet Union developing extensive bioweapons programs.
Despite the 1972 Biological and Toxin Weapons Convention banning bioweapon development, production, and storage, signed by most UN countries, the enduring threat of bioterrorism remains alarming.
Modern bioterrorism
In 1984, the Rajneeshee sect conducted the first known US bioterror attack, contaminating salad bars in The Dalles, Oregon, with Salmonella typhimurium, infecting 751 and hospitalizing 45.
The 2001 US anthrax attacks, where letters containing B anthracis spores were mailed to media and government offices, caused 22 infections, five fatalities and required 30,000 people to undergo antibiotic treatment. The attack fueled widespread fear, prompted biosecurity policy reforms and incurred over $1bn in response costs, highlighting bioterrorism’s social, economic and global security impact.
The US Centers for Disease Control and Prevention classifies biological agents into three categories A, B, and C based on their threat level to public health and national security. Category A agents represent the highest threat due to their high transmissibility, mortality and societal impact, include B. anthracis, Francisella tularensis, Y. pestis, botulinum toxin, smallpox and hemorrhagic fever viruses (Ebola, Marburg).
Category B agents pose a moderate threat, with lower mortality but significant health implications, requiring enhanced diagnostic and surveillance, include Brucella, Clostridium epsilon toxin, Salmonella, Escherichia coli O157:H7, Shigella, Ricin toxin and V cholera.
Viruses are now considered the greatest biothreat in the EU’s expanded list including emerging and re-emerging pathogens—SARS, MERS, WestNile, Mpox and influenza A (H5, H7).
Advancements in biotechnology, CRISPR gene editing and gain-of-function research have reduced barriers to developing bioweapons, raising concerns about non-state actors misusing engineered pathogens or chimera with enhanced virulence or drug resistance. Unlike conventional weapons, BW agents remain silent, invisible and capable of widespread devastation, underscoring the urgency for global biodefense measures.
Biodefense
Biosecurity measures are vital for protecting biological research and mitigating bioterrorism risks. Early detection remains a challenge, as pathogens can spread undetected before symptoms manifest, complicating containment efforts. The Covid-19 pandemic exposed critical gaps in global biodefense, emphasizing the necessity for enhanced surveillance, rapid-response systems and international cooperation. A 2021 Lancet article by Long and Marzi reveals the global biodefense market at $12.2bn in 2019, projected to reach $19.8bn by 2027, growing at a 5.8 percent annual rate.
Strict biosecurity protocols regulate pathogen access, laboratory safety and dual-use research, but inconsistent enforcement and weak compliance mechanisms in many nations create vulnerabilities that could be exploited. A unified global biosecurity framework is essential to ensure scientific advancements benefit humanity, not destruction.
The Biological Weapons Convention prohibits the development, production, acquisition, transfer, stockpiling and use of biological and toxin weapons, yet its enforcement remains inadequate.
Geopolitical tensions complicate biosecurity by fueling mistrust and obstructing global cooperation. Scientific and political debates over SARS-CoV-2’s origins underscore concerns about laboratory safety and accidental pathogen leaks, and the need for stringent oversight in high-containment laboratories.
Safeguarding public health, Nepal’s three-tier health system must enhance surveillance, regulate biotechnology and enforce ethical research standards. Additionally, the Nepali Army and security agencies should develop robust capabilities to detect, prevent and respond to potential bioterrorism threats or bioweapons. This requires coordinated efforts in intelligence gathering, rapid response mechanisms and cross-sectoral collaboration to mitigate hazards and ensure national biosecurity.
Lessons from past pandemics and bioterrorism incidents must inform future biodefense strategies. As Churchill and Gates forewarned, bioterrorism remains an alarming threat. A failure to act now could lead to consequences far more catastrophic than any seen before.
Our gut: A hidden world
“Death sits in the bowels,” and “bad digestion is the root of all evil,” proclaimed Hippocrates, the Greek philosopher and “father of medicine”, in the fourth century BCE. These quotes resonate profoundly in modern science as researchers continue to unveil the critical role the gut plays in both maintaining health and contributing to disease. Far from being just a digestive bowel, our gut harbors a complex and dynamic microbial ecosystem that influences nearly every aspect of our health.
The anatomy
The gut or gastrointestinal (GI) tract spans from the mouth to the rectum, and is crucial for digestion and nutrient absorption. However, its significance goes far beyond breaking down food. The gut is home to approximately 100 trillion microbes—bacteria, archaea, fungi and viruses—that outnumber human host cells by ten-fold. This bustling microbial metropolis, known as the gut microbiome, is often considered an “essential organ” due to its indispensable functions.
Weighing roughly two kilograms—comparable to the human brain size—the gut microbiome contains 150 times more genes than the human genome. Over millennia, these microbes have co-evolved with humans, establishing a symbiosis that profoundly influences our physiology, immune system and even mental health.
A landmark study (Almeida et al 2020) published in Nature Biotechnology highlighted the staggering gut microbiome diversity. The study cataloged 204,938 reference genomes and 170m protein sequences from 4,644 bacterial species found in the human gut. Despite these advances, much of the gut microbiome remains an uncharted territory, with 70 percent of its microbial populations still uncultured in the laboratory and poorly understood.
Diverse, complex microbiota
The gut microbiota (GM) is a highly diverse and intricate microbial community, comprising over 1,000 heterogeneous species dominated by six major phyla, Firmicutes (Clostridium, Lactobacillus, Enterococcus), Bacteroidetes (Bacteroides), Actinobacteria (Bifidobacterium), Proteobacteria (Escherichia coli), Fusobacteria, Verrucomicrobia, and Cyanobacteria. Of these, Firmicutes and Bacteroidetes dominate adult gut microbiota, accounting for 80-90 percent composition.
The dominant fungal species are Candida, Saccharomyces, Malassezia and Cladosporium. Meanwhile, the gut virome, the viral counterpart of the microbiome, is vast and largely uncultivated. Enteroviruses, parechoviruses, and sapoviruses are common residents. A Journal of Clinical Microbiology 2012 case report highlighted the gut virome diversity in stools collected from two healthy infant siblings during their first year of life, identified 15 enteric genera Adenovirus, Aichivirus, Anellovirus, Astrovirus, Bocavirus, Enterovirus, Parechovirus, Picobirnavirus, and Rotavirus. Additionally, the gut DNA viromes of Malawian one-year-old infant twins, with severe acute malnutrition, revealed Anellovirus, Picobirnavirus, and HPeV-1/-6 as the most frequently observed viruses.
Archaea are less diverse but highly conserved, with Methanobrevibacter smithii being the most frequently observed species across all six continents.
Each individual’s GM is a unique microbial signature, shaped by genetics, immune function, diet, lifestyle, environment, epigenetics and early microbial exposure during birth and breastfeeding. These microbes colonize different GI tract sections, with the highest biomass found in the caecum and proximal colon.
Health guardians
GM performs crucial functions for maintaining health. In digestion and metabolism, gut microbes break down complex carbohydrates, synthesize vitamins such as B and K (via Bifidobacterium, Lactobacillus, Salmonella, Streptococcus, Clostridia, and Listeria), and produce short-chain fatty acids (SCFAs) like butyrate, which nourish colonic cells and regulate inflammation.
While humans cannot digest fiber, bacteria possess glycoside hydrolases/ polysaccharide lysases that ferment plant polysaccharides. Gut bacteria Eubacterium, Roseburia, Faecalibacterium and Coprococcus ferment indigestible fibers like resistant starches, and cellulose, generating butyrate, provides energy to colonocytes. Butyrate enhances bowel health by regulating colonic motility, improving blood flow and preventing pathogen overgrowth. GM Bacillus subtilis and E. coli synthesize riboflavin (vitamin B2), essential for cellular metabolism. With 70 percent of the immune system in the gut, microbes train immune cells to differentiate pathogens, ensuring immune balance. Furthermore, they strengthen the intestinal barrier, preventing harmful pathogens and toxins from entering the bloodstream.
Through the gut-brain axis, they influence mood, cognition and behavior, impacting conditions like anxiety and depression. Maintaining a healthy balance of GM, known as ‘normobiosis’, is crucial for overall well-being. Disruptions to this balance, ‘dysbiosis’, fosters pathogen overgrowth triggering health issues.
Declining diversity
Modern lifestyles and urbanization have significantly reduced GM diversity, impacting health. Processed diets, irrational antimicrobial use, sedentary lifestyles, high salt/protein intake and limited exposure to natural environments have caused a multigenerational loss of beneficial microbial signatures, key for immune resilience. A 2024 study in Kazakhstan revealed stark differences in gut diversity between urban and rural populations. Urban microbiomes showed reduced diversity, elevated Firmicutes/Bacteroidetes ratios and higher prevalence of Coprococcus and Parasutterella. Rural populations exhibited greater microbial diversity, with abundant Ligilactobacillus and Paraprevotella, correlating with their fiber-rich diets. Interestingly, a Nepali study (Jha et al 2018) found traditional Himalayan populations (Chepang, Raute, Raji, and Tharu) had distinct microbiome signatures compared to Americans, emphasizing lifestyles impact on gut diversity.
This GM diversity depletion is linked to autoimmune diseases and chronic inflammation. Dysbiosis is implicated in obesity where excessive Firmicutes enhance fat absorption. Inflammatory bowel disease (IBD) (Crohn’s disease, Ulcerative colitis), features reduced alpha diversity and shifts favoring pathogenic Gamma-proteobacteria. Colorectal cancer patients exhibit harmful bacteria, such as Fusobacterium nucleatum, genotoxic E. coli, Enterotoxigenic Bacteroides fragilis, produce metabolites fostering tumorigenesis. Dysbiosis also influences metabolic disorders (diabetes) and neurodegenerative diseases (Alzheimer’s, Parkinson's) through inflammation and the gut-brain axis.
Advancements
Advancements in gut microbiome research herald a new era of personalized medicine. Probiotics/prebiotics restore microbial balance by enhancing beneficial GM, while fiber-rich diets and healthy lifestyles promote gut health reducing inflammation. Conversely, ultra-processed foods, artificial sweeteners and emulsifiers disrupt this balance, decreasing diversity and driving inflammation. Innovations like fecal microbiota transplant treat C. difficile infections and hold promise for IBD.
Despite progress, gut microbiome research is still in its infancy, with challenges in decoding complex host-microbe interactions. Investigating gut microbial signatures of exceptional mountain climbers, like Sherpas, and ethnic Nepali communities could lead to personalized therapies. Technologies like metagenomics/metabolomics offer breakthroughs in diagnostics and therapies. Deepening our understanding of this hidden world within us can unlock new avenues to enhance well-being and resilience.
HMPV: A known virus, not a mystery
Recent reports of a Human Metapneumovirus (HMPV) outbreak in China have triggered global concerns, with echoes of the early Covid-19 pandemic raising speculation about a potential health emergency. However, HMPV is not a new or mysterious virus. It has been well-documented for decades as a significant cause of respiratory illness in children, elderly and immunocompromised individuals.
Identified in 2001 at Erasmus Medical Center in the Netherlands, HMPV was initially isolated from children with respiratory illnesses. Published in Nature Medicine, this study indicated all Dutch children were exposed to HMPV by the age of five. Retrospective analyses, however, suggest HMPV has been circulating in humans for 50 years.
HMPV belongs to the Pneumoviridae family along with respiratory syncytial virus (RSV) and the Metapneumovirus genus. This enveloped, single-stranded negative-sense RNA virus has two genetic lineages, A and B, further divided into six sublineages: A1, A2.1, A2.2.1, A2.2.2, B1 and B2. Emerging sublineages A2.2.1 and A2.2.2, were recently identified in pediatric respiratory infections in South India, as reported by the International Society of Infectious Diseases in 2025.
A Virology Journal 2009 genetic study by Vanderbilt University suggests HMPV diverged from Avian Metapneumovirus 200–400 years ago via zoonotic spillover from an avian reservoir, with phylogenetic evidence indicating a spillover event around 200 years ago, emphasizing HMPV’s long-standing presence in human populations.
Symptoms, risk groups and treatment
HMPV is a common etiological agent of respiratory tract infections, affecting infants, children under 15, the elderly, and immunocompromised individuals. Nearly all children are exposed by age five, with reinfections occurring throughout life. According to the US Centers for Disease Control and Prevention (CDC), it spreads via respiratory droplets, close contact, or contaminated surfaces, similar to the transmission of SARS-CoV-2, with an incubation period of 3–6 days. Symptoms vary from mild cough, nasal congestion, fever, and breath shortness to severe pneumonia, bronchiolitis, asthma exacerbations, especially in high-risk groups.
Infants and young children are prone to severe bronchiolitis and pneumonia. The elderly, often with comorbidities like asthma, may experience complications. Immunocompromised individuals face prolonged or severe illness, and pregnant women are at risk of respiratory complications that could affect both maternal and fetal health.
No specific antiviral treatment or vaccine exists for HMPV. Management relies on supportive care, supplemental oxygen, antipyretics and intravenous hydration when needed.
Seasonal outbreaks
HMPV is a seasonal respiratory virus, primarily circulating during late winter and early spring in temperate regions, similar to influenza and RSV. Recent reports of increased cases in China and parts of Asia align with this seasonal pattern. US CDC data also highlight annual outbreaks during these months, influenced by climatic conditions.
Despite comparisons to the Covid-19 pandemic, HMPV is not a novel virus. Identified over two decades back, it has been extensively studied, with over 300 PubMed scientific articles available. While it causes localized outbreaks, its transmission dynamics and clinical severity do not indicate pandemic potential. For instance, HMPV was the predominant virus during the 2002–2003 winter in Norwegian children hospitalized for respiratory infections, as reported in The Pediatric Infectious Disease Journal. Severe pneumonia occurred in some cases, but widespread outbreaks have remained limited to specific populations.
HMPV outbreaks have been documented globally, including Israel (2003), Japan (2003–2004), South Africa (2009-2013), Nicaragua (2011-2016), Western Sydney (2018), South Korea (2022), India (2022), China (2017-2023) and various regions. In Pakistan, HMPV accounted for 5–7 percent of pneumonia admissions in children at Aga Khan University Hospital (2009–2012). HMPV causes 5–10 percent of pediatric acute respiratory infections (ARIs) hospitalizations and is the second most common viral pathogen in certain settings. ARIs are a major global public health problem, causing significant morbidity and mortality, particularly in children.
A 2019 study at Nepal’s Kanti Children’s Hospital revealed a prevalence of 13 percent among children with ARIs, with infections more frequent in those under three years old (22 percent). Symptoms like cough and fever were universally observed.
Besides, data from Nepal’s Sarlahi district (2011–2014) detected HMPV in five percent of infants, identifying three genotypes (A2, B1, B2). A recent Chinese CDC analysis ranked HMPV second among 11 respiratory viruses affecting children under 15 years, with a positivity rate of 6.2 percent in influenza-like illness.
These findings reflect a seasonal uptick, not an unprecedented surge. Factors like colder weather and increased indoor crowding contribute to HMPV’s seasonal prevalence.
Covid-19 lessons
The Covid-19 pandemic highlighted the importance of preparedness, evidence-based communication and robust public health strategies in managing infectious disease outbreaks. While HMPV does not pose the same threat as Covid-19, its current attention emphasizes the need to apply these lessons. Strengthened surveillance systems are essential for early detection, while public education can counter misinformation, reduce anxiety and encourage preventive behaviors. Investment in research on HMPV’s pathogenesis, treatments and vaccine development is key to mitigating its long-term impacts and bolstering public health resilience.
Precautions
The rise in HMPV cases in China and India warrants vigilance but not alarm. Vulnerable populations—infants, rural children, immunocompromised individuals—are particularly at risk, in regions with limited healthcare resources like Nepal. Preventive measures, supportive care and community-driven initiatives are critical to minimizing HMPV’s burden.
Between 2011 and 2014, HMPV infections in rural southern Nepal were associated with adverse outcomes, including an increased risk of small-for-gestational-age births in pregnant women. Interventions targeting febrile respiratory illness in pregnancy could improve maternal and neonatal health in resource-limited settings.
Hygiene practices, regular handwashing and respiratory etiquette, alongside isolation during illness, can reduce HMPV transmission. Enhanced diagnostic capabilities and heightened awareness will support disease management and safeguard at-risk groups.
Policymakers, healthcare providers and community leaders must collaborate to strengthen surveillance systems, improve diagnostics and develop effective preventive strategies. Public health messaging should prioritize education and reassurance, focusing on practical actions to protect vulnerable populations. By taking informed and measured steps, HMPV’s impact can be effectively mitigated, fostering resilience against future viral outbreaks.
The author is a researcher with a PhD degree at Nexus Institute of Research and Innovation